Bariatric Surgery (Weight Loss Suregery ) Treatments
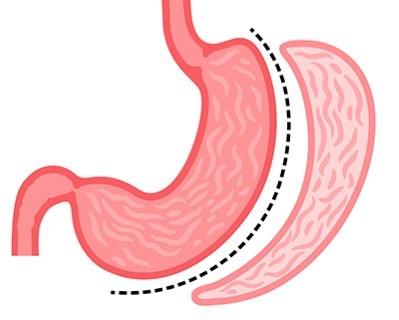
Sleeve Gastrectomy
- Purpose: Reduces the size of the stomach to limit food intake and promote weight loss.
- Procedure: A large portion of the stomach is removed, creating a sleeve-shaped stomach.
-
Note: The information provided here applies to elective Sleeve Gastrectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Sleeve Gastrectomy is typically performed as an inpatient procedure. This major weight-loss surgery requires patients to be admitted to the hospital for close monitoring before, during, and after the procedure. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or nutrient deficiencies.Hospital Stay Duration
Patients undergoing Sleeve Gastrectomy usually stay in the hospital for 2 to 3 days. The initial post-operative period involves monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after Sleeve Gastrectomy surgery. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress.Pre-procedure Preparation
Preparation for Sleeve Gastrectomy typically involves several steps, including dietary adjustments, weight loss, and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet for a few weeks before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests and imaging studies, is conducted to plan the surgery.Procedure Duration
The Sleeve Gastrectomy procedure typically takes 1 to 2 hours. The surgery involves removing approximately 75-80% of the stomach, leaving a tube-shaped stomach or "sleeve." This significantly reduces the stomach's capacity, leading to reduced food intake and promoting weight loss.Recovery Time
Recovery from Sleeve Gastrectomy surgery can take several weeks. Most patients are encouraged to engage in light activities, such as walking, soon after discharge, but full recovery, including a return to work and more strenuous activities, may take up to 4 to 6 weeks. Patients will need to follow a special diet, starting with liquids and gradually progressing to pureed and then solid foods. Regular follow-up appointments and participation in a bariatric surgery support program are essential for monitoring weight loss progress and addressing any nutritional needs or complications.Estimated Cost
The cost of Sleeve Gastrectomy surgery can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Sleeve Gastrectomy involves a significant focus on diet and lifestyle changes. Patients will need to follow a structured eating plan, including taking vitamin and mineral supplements to prevent deficiencies. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications. Patients will also receive guidance on incorporating physical activity into their routine to support long-term weight loss and health. Psychological support or counseling may be recommended to help patients adjust to the changes following surgery and to address any emotional or behavioral issues related to eating.
_20240719132648774823__0.webp)
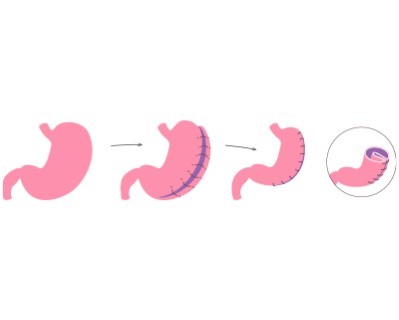
Endoscopic Sleeve Gastroplasty (ESG)
- Purpose: Reduces the size of the stomach to promote weight loss using a non-surgical approach.
- Procedure: An endoscope is used to place sutures in the stomach to create a sleeve-like shape.
-
Note: The information provided here applies to elective Endoscopic Sleeve Gastroplasty (ESG) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the procedure and recovery process.
Inpatient/Outpatient
Endoscopic Sleeve Gastroplasty (ESG) is typically performed as an outpatient procedure. This minimally invasive weight-loss procedure does not require surgical incisions, allowing most patients to return home the same day. The procedure is usually conducted in a hospital or specialized clinic, where patients are monitored for a few hours afterward to ensure they recover safely.Hospital Stay Duration
Patients undergoing ESG generally do not require an overnight hospital stay. The entire process, including preparation, the procedure itself, and post-procedure monitoring, typically takes about 4 to 6 hours. After the procedure, patients are observed to ensure they are stable and can usually be discharged within a few hours.Type of Anesthesia
ESG is typically performed under general anesthesia or deep sedation, ensuring that the patient is comfortable and unconscious during the procedure. This allows the endoscopist to safely perform the procedure, which involves using an endoscope to suture the stomach and create a sleeve-like shape, reducing its capacity.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least a few days after ESG. This allows time for initial recovery and monitoring for any early complications, such as pain, nausea, or vomiting. Most patients can resume normal activities within a week, but they should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for ESG typically involves following a liquid or low-calorie diet for a few days to a week before the procedure to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during the procedure. The healthcare provider will provide specific pre-procedure instructions, including any necessary tests or evaluations.Procedure Duration
The ESG procedure typically takes about 60 to 90 minutes. During the procedure, an endoscope equipped with a suturing device is inserted through the mouth and into the stomach. The endoscopist then places a series of stitches to reduce the size of the stomach, creating a sleeve-like shape that limits food intake.Recovery Time
Recovery from ESG is generally quicker than traditional surgical weight-loss procedures. Most patients can resume light activities within a few days, but it is recommended to follow a gradual return to normal activities, including exercise, over the next few weeks. Patients will need to adhere to a special post-procedure diet, starting with liquids and gradually progressing to pureed and then solid foods over several weeks. Full recovery and adaptation to the new eating pattern may take several weeks.Estimated Cost
The cost of ESG can vary depending on the clinic, geographic location, and the specifics of the patient’s condition. ESG is generally less expensive than traditional bariatric surgery, but costs can still be significant. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for ESG involves a structured diet and lifestyle changes. Patients will begin with a liquid diet, followed by pureed foods, and eventually transition to solid foods over several weeks. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications. Patients will also receive guidance on incorporating physical activity and making long-term dietary changes to support weight loss and overall health. Psychological support or counseling may be recommended to help patients adjust to the changes following ESG and to address any emotional or behavioral issues related to eating.
_20240719132800044252__0.webp)
Gastric Bypass Surgery (Roux-en-Y)
Purpose: To promote weight loss by reducing the size of the stomach and bypassing a portion of the small intestine.
Procedure: The stomach is divided into a small upper pouch and a larger lower pouch, and the small intestine is rearranged to connect to both parts.
Note: The information provided here is applicable to elective Roux-en-Y Gastric Bypass procedures performed under standard conditions. However, details may vary depending on individual patient factors such as the presence of obesity-related comorbidities, patient tolerance, or complications that may arise during or after surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also impact the surgery and recovery process.
Hospitalization/Clinic: Roux-en-Y Gastric Bypass surgery is typically performed as an inpatient procedure. This major weight loss surgery requires hospitalization for close monitoring before, during, and after the surgery. Most patients need to stay in the hospital to ensure proper recovery and to monitor potential complications such as bleeding, infection, or nutritional deficiencies.
Hospital Stay Duration: Patients undergoing Gastric Bypass Surgery typically stay in the hospital for 2 to 3 days. The initial postoperative period involves monitoring in a special care unit to observe complications and manage pain and recovery. If the patient has other underlying conditions or if complications arise during recovery, the hospital stay may be extended.
Type of Anesthesia: The procedure is performed under general anesthesia, which means the patient will be completely unconscious during the surgery. General anesthesia ensures that the patient remains comfortable and immobile, allowing the surgical team to perform the procedure safely and effectively.
Postoperative Travel: Patients are generally advised to avoid traveling, especially long-distance or air travel, for at least 2 to 4 weeks after Gastric Bypass Surgery. This period allows for initial healing and recovery. The healthcare provider will offer specific advice on travel and activity levels based on the patient's recovery process.
Preoperative Preparation: Preparation for Gastric Bypass Surgery typically involves several steps, including dietary modifications, weight loss, and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet several weeks before the surgery to reduce liver size and improve surgical outcomes. Patients may also need to discontinue certain medications, particularly blood thinners, to reduce the risk of bleeding. A thorough preoperative assessment, including blood tests and imaging studies, is conducted to plan the surgery.
Procedure Duration: The Gastric Bypass Surgery procedure generally takes 2 to 4 hours. The surgery involves creating a small pouch from the upper part of the stomach and connecting it directly to the small intestine, bypassing a large portion of the stomach and the initial part of the small intestine. This reduces stomach capacity and limits nutrient absorption, leading to significant weight loss.
Recovery Time: Recovery from Gastric Bypass Surgery can take several weeks. Most patients are encouraged to engage in light activities such as walking after discharge, but full recovery, return to work, and resumption of more strenuous activities may take 4 to 6 weeks. Patients should follow a specific diet starting with liquids, then progressing to pureed foods, and finally solid foods. Regular follow-up appointments and participation in a bariatric surgery support program are crucial for monitoring weight loss progress and addressing nutritional needs or complications.
Estimated Cost: The cost of Gastric Bypass Surgery can vary widely depending on the hospital, geographic location, and patient-specific factors. Patients should contact their healthcare providers or hospitals directly for accurate cost information.
Postoperative Care: Postoperative care after Gastric Bypass Surgery focuses heavily on dietary and lifestyle changes. Patients must adhere to a structured meal plan that includes vitamin and mineral supplements (such as vitamin B12, iron, calcium, and vitamin D) to prevent nutritional deficiencies. Regular follow-up appointments are critical to monitor weight loss, nutritional status, and potential complications such as dumping syndrome or anastomotic leaks. Patients will also receive guidance on incorporating physical activity into their routines to support long-term weight loss and health. Psychological support or counseling may be recommended to help adapt to postoperative changes and address emotional or behavioral issues related to eating.
_20240719132859436017__0.webp)
Adjustable Gastric Banding (Lap-Band)
Purpose: To reduce the size of the stomach and restrict food intake.
Procedure: An adjustable band is placed around the upper part of the stomach to create a small pouch.
Note: The information provided here is applicable to elective Adjustable Gastric Banding (Lap-Band) procedures performed under standard conditions. However, details may vary depending on individual patient factors such as the presence of obesity-related comorbidities, patient tolerance, or complications that may arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for band adjustments can also affect the surgery and recovery process.
Hospitalization/Clinic: Adjustable Gastric Banding (Lap-Band) is typically performed as an outpatient procedure. This minimally invasive weight loss surgery usually allows patients to return home on the same day. However, if the patient has other health issues, an overnight stay for closer monitoring may be recommended.
Hospital Stay Duration: Patients undergoing Adjustable Gastric Banding typically do not stay in the hospital overnight. The procedure generally lasts 1 to 2 hours, including preparation and recovery time. After the procedure, patients are observed for a few hours to ensure recovery from anesthesia and to determine if they are ready for discharge.
Type of Anesthesia: The procedure is performed under general anesthesia, which means the patient will be completely unconscious during the surgery. General anesthesia ensures that the patient remains comfortable and immobile, allowing the surgical team to perform the procedure safely and effectively.
Postoperative Travel: Patients are generally advised to avoid traveling, especially long-distance or air travel, for at least a few days after Adjustable Gastric Banding. This period is necessary for initial recovery and monitoring of early complications (such as pain, nausea, or vomiting). Most patients can return to normal activities within a week, but they should follow their healthcare provider’s specific recommendations regarding travel and activity levels.
Preoperative Preparation: Preparation for Adjustable Gastric Banding usually involves several steps, including dietary changes and lifestyle modifications to optimize health before surgery. Patients are often instructed to follow a liquid or low-calorie diet several days to a week before the surgery to reduce liver size and improve surgical outcomes. Patients may also need to discontinue certain medications, particularly blood thinners, to reduce the risk of bleeding. A comprehensive preoperative assessment, including blood tests and imaging studies, is conducted to plan the surgery.
Procedure Duration: The Adjustable Gastric Banding procedure typically takes 1 to 2 hours. During the procedure, an adjustable silicone band is placed around the upper part of the stomach to create a small pouch that restricts food intake. The tightness of the band can be adjusted over time through a port placed under the skin, allowing for personalized weight loss management.
Recovery Time: Recovery from Adjustable Gastric Banding is generally faster than more invasive weight loss surgeries. Most patients can return to light activities within a few days, but vigorous exercise should be avoided. Patients should follow a specific diet that starts with liquids, then progresses to pureed foods, and finally solid foods. Full recovery and adjustment to new eating habits may take several weeks to a few months.
Estimated Cost: The cost of Adjustable Gastric Banding can vary widely depending on the hospital, geographic location, and patient-specific factors. Patients should contact their healthcare providers or hospitals directly for accurate cost information.
Postoperative Care: Postoperative care after Adjustable Gastric Banding involves regular follow-up appointments to monitor weight loss, adjust the band as needed, and address potential complications. Patients should adhere to a structured meal plan to ensure proper nutrition and prevent overeating or discomfort. Regular adjustments to the band may be necessary to optimize weight loss. Patients will also receive guidance on incorporating physical activity and long-term dietary changes into their routines to support sustained weight loss and health. Psychological support or counseling may be recommended to help adapt to postoperative changes and address any emotional or behavioral issues related to eating.
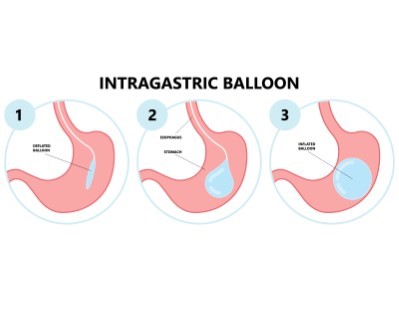
Intragastric Balloon
- Purpose: Reduces food intake by occupying space in the stomach.
- Procedure: A b
Note: The information provided here applies to elective Intragastric Balloon procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the procedure. The patient’s overall health, the complexity of the procedure, and the need for balloon adjustments or removal can also influence the procedure and recovery process.
Inpatient/Outpatient
The Intragastric Balloon procedure is typically performed as an outpatient procedure. This non-surgical weight-loss method allows most patients to return home the same day. The procedure is usually conducted in a hospital or specialized clinic, where patients are monitored for a few hours after the balloon is placed to ensure they recover safely and are stable for discharge.Hospital Stay Duration
Patients undergoing the Intragastric Balloon procedure generally do not require an overnight hospital stay. The procedure itself usually takes about 20 to 30 minutes, followed by a short recovery period to ensure there are no immediate complications, such as nausea or discomfort. Most patients can go home within a few hours after the procedure.Type of Anesthesia
The procedure is performed under conscious sedation or light anesthesia, which helps the patient remain relaxed and comfortable while allowing the endoscopist to place the balloon in the stomach. Local anesthesia may also be used to numb the throat, reducing discomfort during the insertion of the endoscope.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least a few days after the procedure to allow time for initial recovery and to monitor for any early complications, such as nausea or vomiting. Most patients can resume normal activities within a week, but they should follow specific recommendations from their healthcare provider regarding travel and activity levels.Pre-procedure Preparation
Preparation for the Intragastric Balloon procedure typically involves dietary adjustments, such as fasting for 12 hours before the procedure to ensure the stomach is empty. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding or complications during the procedure. The healthcare provider will provide specific pre-procedure instructions tailored to the patient’s needs.Procedure Duration
The Intragastric Balloon procedure typically takes about 20 to 30 minutes. During the procedure, an endoscope is passed through the mouth and into the stomach, and the balloon is then inserted and filled with saline solution or gas until it reaches the desired size. The balloon takes up space in the stomach, helping to reduce food intake and promote weight loss.Recovery Time
Recovery from the Intragastric Balloon procedure is generally quick, with most patients able to resume light activities within a few days. However, patients may experience nausea, vomiting, or discomfort for the first few days after the procedure as the stomach adjusts to the presence of the balloon. A special diet is recommended immediately after the procedure, starting with liquids and gradually progressing to soft foods and then regular foods. Full adaptation to the balloon and the new eating pattern may take a few weeks.Estimated Cost
The cost of the Intragastric Balloon procedure can vary depending on the clinic, geographic location, and the specifics of the patient’s condition. Costs typically include the initial placement of the balloon, follow-up appointments, and the eventual removal of the balloon after 6 to 12 months. For accurate cost information, patients should contact their healthcare provider or treatment center directly.Post-procedure Care
Post-procedure care for the Intragastric Balloon involves regular follow-up appointments to monitor weight loss, nutritional status, and any potential complications. Patients will need to follow a structured eating plan to ensure proper nutrition and to maximize weight loss while the balloon is in place. The balloon is usually removed after 6 to 12 months through a similar endoscopic procedure. Patients will also receive guidance on incorporating physical activity and making long-term dietary changes to support sustained weight loss and overall health. Psychological support or counseling may be recommended to help patients adjust to the changes following the procedure and to address any emotional or behavioral issues related to eating. Balloon is inserted into the stomach and filled with saline to reduce hunger.
_20240719133045829849__0.webp)
Mini Gastric Bypass (MGB)
- Purpose: Simplifies gastric bypass surgery with a shorter procedure and similar outcomes.
- Procedure: Creates a small stomach pouch and bypasses a portion of the small intestine.
-
Note: The information provided here applies to elective Mini Gastric Bypass (MGB) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Mini Gastric Bypass (MGB) is typically performed as an inpatient procedure. This weight-loss surgery requires patients to be admitted to the hospital for close monitoring before, during, and after the procedure. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or nutrient deficiencies.Hospital Stay Duration
Patients undergoing Mini Gastric Bypass usually stay in the hospital for 2 to 3 days. The initial post-operative period involves monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after Mini Gastric Bypass surgery. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress.Pre-procedure Preparation
Preparation for Mini Gastric Bypass typically involves several steps, including dietary adjustments, weight loss, and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet for a few weeks before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests and imaging studies, is conducted to plan the surgery.Procedure Duration
The Mini Gastric Bypass procedure typically takes 1.5 to 2.5 hours. The surgery involves creating a small gastric pouch from the upper section of the stomach and connecting it to a loop of the small intestine, bypassing a portion of the stomach and the first part of the small intestine. This reduces the stomach’s capacity and limits nutrient absorption, leading to significant weight loss.Recovery Time
Recovery from Mini Gastric Bypass surgery can take several weeks. Most patients are encouraged to engage in light activities, such as walking, soon after discharge, but full recovery, including a return to work and more strenuous activities, may take up to 4 to 6 weeks. Patients will need to follow a special diet, starting with liquids and gradually progressing to pureed and then solid foods. Regular follow-up appointments and participation in a bariatric surgery support program are essential for monitoring weight loss progress and addressing any nutritional needs or complications.Estimated Cost
The cost of Mini Gastric Bypass surgery can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Mini Gastric Bypass involves significant focus on diet and lifestyle changes. Patients will need to follow a structured eating plan, including taking vitamin and mineral supplements to prevent deficiencies, such as vitamin B12, iron, calcium, and vitamin D. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications, such as dumping syndrome or anastomotic ulcers. Patients will also receive guidance on incorporating physical activity into their routine to support long-term weight loss and health. Psychological support or counseling may be recommended to help patients adjust to the changes following surgery and to address any emotional or behavioral issues related to eating.
Gastric Plication
- Purpose: Reduces the size of the stomach without removing any part of it.
- Procedure: Folds the stomach inward and sutures it to reduce its volume.
-
Note: The information provided here applies to elective Gastric Plication procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Gastric Plication is typically performed as an inpatient procedure. This minimally invasive weight-loss surgery usually requires patients to be admitted to the hospital for close monitoring before, during, and after the procedure. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or nutrient deficiencies.Hospital Stay Duration
Patients undergoing Gastric Plication usually stay in the hospital for 1 to 2 days. The initial post-operative period involves monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 1 to 2 weeks after Gastric Plication surgery. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress.Pre-procedure Preparation
Preparation for Gastric Plication typically involves several steps, including dietary adjustments and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet for a few days to a week before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests and imaging studies, is conducted to plan the surgery.Procedure Duration
The Gastric Plication procedure typically takes 1 to 2 hours. The surgery involves folding the stomach in on itself and suturing the folds to reduce the stomach’s volume by about 70%, thereby limiting food intake and promoting weight loss. Unlike other bariatric procedures, no part of the stomach is removed, and no foreign objects, such as bands, are implanted.Recovery Time
Recovery from Gastric Plication surgery is generally quicker than other bariatric surgeries. Most patients can return to light activities within a few days, but it is recommended to avoid strenuous exercise for several weeks. Patients will need to follow a special post-procedure diet, starting with liquids and gradually progressing to pureed and then solid foods over several weeks. Full recovery and adaptation to the new eating pattern may take several weeks to a few months.Estimated Cost
The cost of Gastric Plication can vary depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Gastric Plication involves regular follow-up appointments to monitor weight loss, nutritional status, and any potential complications. Patients will need to follow a structured eating plan to ensure proper nutrition and maximize weight loss. Regular physical activity is encouraged to support long-term weight loss and overall health. Patients will also receive guidance on incorporating healthy lifestyle changes and may benefit from psychological support or counseling to address any emotional or behavioral issues related to eating and weight loss.
Revisional Bariatric Surgery
- Purpose: Corrects or improves the outcomes of previous bariatric surgery.
- Procedure: Varies depending on the initial surgery and required adjustments.
-
Note: The information provided here applies to elective Revisional Bariatric Surgery procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the reason for revision, the type of previous bariatric surgery, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the revision, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Revisional Bariatric Surgery is typically performed as an inpatient procedure due to its complexity. This type of surgery is often more complicated than the initial bariatric procedure, requiring patients to be admitted to the hospital for close monitoring before, during, and after the surgery. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or issues related to the initial bariatric surgery.Hospital Stay Duration
Patients undergoing Revisional Bariatric Surgery usually stay in the hospital for 2 to 4 days, depending on the complexity of the surgery and the patient’s overall health. The initial post-operative period involves close monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after Revisional Bariatric Surgery. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress and the complexity of the revision.Pre-procedure Preparation
Preparation for Revisional Bariatric Surgery typically involves several steps, including dietary adjustments, weight loss, and lifestyle changes to optimize health before surgery. Patients may be instructed to follow a liquid or low-calorie diet for a few weeks before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests, imaging studies, and possibly an evaluation of the initial bariatric procedure, is conducted to plan the revision surgery.Procedure Duration
The duration of Revisional Bariatric Surgery varies depending on the type of revision being performed and the complexity of the case. The procedure can take anywhere from 2 to 4 hours or more. The surgery may involve correcting issues from the initial bariatric procedure, converting one type of bariatric surgery to another, or addressing complications such as weight regain, nutritional deficiencies, or mechanical problems with the original surgery.Recovery Time
Recovery from Revisional Bariatric Surgery can take several weeks to a few months, depending on the complexity of the revision and the patient’s overall health. Most patients are encouraged to engage in light activities, such as walking, soon after discharge, but full recovery, including a return to work and more strenuous activities, may take up to 6 to 8 weeks. Patients will need to follow a special post-procedure diet, starting with liquids and gradually progressing to pureed and then solid foods. Regular follow-up appointments are essential for monitoring recovery, weight loss, and addressing any nutritional needs or complications.Estimated Cost
The cost of Revisional Bariatric Surgery can vary widely depending on the hospital, geographic location, and the complexity of the revision. Revisional procedures are often more expensive than initial bariatric surgeries due to their complexity. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Revisional Bariatric Surgery involves significant focus on diet, lifestyle changes, and ongoing monitoring. Patients will need to follow a structured eating plan, including taking vitamin and mineral supplements to prevent deficiencies. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications specific to the revision. Patients will also receive guidance on incorporating physical activity into their routine to support long-term weight loss and health. Psychological support or counseling may be recommended to help patients adjust to the changes following surgery and to address any emotional or behavioral issues related to eating and weight loss.
_20240719153213398470__0.webp)
Vertical Sleeve Gastrectomy (VSG)
- Purpose: Reduces stomach size to promote weight loss.
- Procedure: Removes a large portion of the stomach, leaving a tube-shaped section.
-
Note: The information provided here applies to elective Vertical Sleeve Gastrectomy (VSG) procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Vertical Sleeve Gastrectomy (VSG) is typically performed as an inpatient procedure. This major weight-loss surgery requires patients to be admitted to the hospital for close monitoring before, during, and after the procedure. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or nutrient deficiencies.Hospital Stay Duration
Patients undergoing VSG usually stay in the hospital for 2 to 3 days. The initial post-operative period involves monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after VSG surgery. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress.Pre-procedure Preparation
Preparation for VSG typically involves several steps, including dietary adjustments, weight loss, and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet for a few weeks before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests and imaging studies, is conducted to plan the surgery.Procedure Duration
The VSG procedure typically takes 1 to 2 hours. The surgery involves removing approximately 75-80% of the stomach, leaving a tube-shaped stomach or "sleeve." This significantly reduces the stomach's capacity, leading to reduced food intake and promoting weight loss. Unlike other bariatric procedures, VSG does not involve rerouting the intestines.Recovery Time
Recovery from VSG surgery can take several weeks. Most patients are encouraged to engage in light activities, such as walking, soon after discharge, but full recovery, including a return to work and more strenuous activities, may take up to 4 to 6 weeks. Patients will need to follow a special diet, starting with liquids and gradually progressing to pureed and then solid foods. Regular follow-up appointments and participation in a bariatric surgery support program are essential for monitoring weight loss progress and addressing any nutritional needs or complications.Estimated Cost
The cost of VSG surgery can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for VSG involves significant focus on diet and lifestyle changes. Patients will need to follow a structured eating plan, including taking vitamin and mineral supplements to prevent deficiencies, such as vitamin B12, iron, calcium, and vitamin D. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications. Patients will also receive guidance on incorporating physical activity into their routine to support long-term weight loss and health. Psychological support or counseling may be recommended to help patients adjust to the changes following surgery and to address any emotional or behavioral issues related to eating.
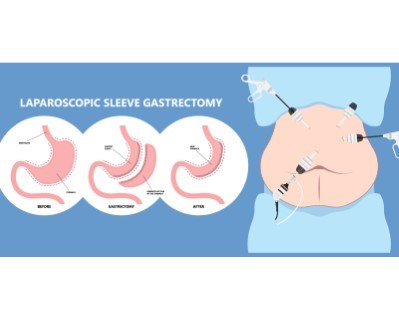
Laparoscopic Sleeve Gastrectomy
- Purpose: Reduces the size of the stomach to limit food intake and promote weight loss.
- Procedure: A large portion of the stomach is removed using a laparoscope, creating a sleeve-shaped stomach.
-
Note: The information provided here applies to elective Laparoscopic Sleeve Gastrectomy procedures under standard conditions. However, specifics may vary depending on individual patient factors, such as the presence of obesity-related comorbidities, patient tolerance, or any complications that might arise during or after the surgery. The patient’s overall health, the complexity of the procedure, and the need for additional interventions can also influence the surgery and recovery process.
Inpatient/Outpatient
Laparoscopic Sleeve Gastrectomy is typically performed as an inpatient procedure. This minimally invasive weight-loss surgery requires patients to be admitted to the hospital for close monitoring before, during, and after the procedure. Most patients will require a hospital stay to ensure proper recovery and to monitor for any potential complications, such as bleeding, infection, or nutrient deficiencies.Hospital Stay Duration
Patients undergoing Laparoscopic Sleeve Gastrectomy usually stay in the hospital for 2 to 3 days. The initial post-operative period involves monitoring in a specialized care unit to observe for any complications and to manage pain and recovery. The length of stay may be extended if the patient has other underlying conditions or if complications arise during recovery.Type of Anesthesia
The procedure is performed under general anesthesia, meaning the patient will be fully unconscious during the surgery. General anesthesia is necessary to keep the patient comfortable and still, allowing the surgical team to perform the procedure safely and effectively.Travel After Procedure
Patients are generally advised to avoid travel, particularly long-distance or air travel, for at least 2 to 4 weeks after Laparoscopic Sleeve Gastrectomy. This period allows time for initial recovery and healing. The healthcare provider will provide specific recommendations regarding travel and activity levels based on the patient’s recovery progress.Pre-procedure Preparation
Preparation for Laparoscopic Sleeve Gastrectomy typically involves several steps, including dietary adjustments, weight loss, and lifestyle changes to optimize health before surgery. Patients are usually instructed to follow a liquid or low-calorie diet for a few weeks before surgery to reduce the size of the liver and improve surgical outcomes. Patients may also need to stop taking certain medications, particularly blood thinners, as directed by their healthcare provider to minimize the risk of bleeding during surgery. A comprehensive pre-operative assessment, including blood tests and imaging studies, is conducted to plan the surgery.Procedure Duration
The Laparoscopic Sleeve Gastrectomy procedure typically takes 1 to 2 hours. The surgery involves removing approximately 75-80% of the stomach, leaving a tube-shaped stomach or "sleeve." This significantly reduces the stomach's capacity, leading to reduced food intake and promoting weight loss. The laparoscopic approach involves small incisions and the use of a camera and specialized instruments, which typically results in shorter recovery times and less post-operative pain compared to open surgery.Recovery Time
Recovery from Laparoscopic Sleeve Gastrectomy can take several weeks. Most patients are encouraged to engage in light activities, such as walking, soon after discharge, but full recovery, including a return to work and more strenuous activities, may take up to 4 to 6 weeks. Patients will need to follow a special diet, starting with liquids and gradually progressing to pureed and then solid foods. Regular follow-up appointments and participation in a bariatric surgery support program are essential for monitoring weight loss progress and addressing any nutritional needs or complications.Estimated Cost
The cost of Laparoscopic Sleeve Gastrectomy can vary widely depending on the hospital, geographic location, and the specifics of the patient’s condition. For accurate cost information, patients should contact their healthcare provider or hospital directly.Post-procedure Care
Post-procedure care for Laparoscopic Sleeve Gastrectomy involves significant focus on diet and lifestyle changes. Patients will need to follow a structured eating plan, including taking vitamin and mineral supplements to prevent deficiencies, such as vitamin B12, iron, calcium, and vitamin D. Regular follow-up appointments are crucial to monitor weight loss, nutritional status, and any potential complications. Patients will also receive guidance on incorporating physical activity into their routine to support long-term weight loss and health. Psychological support or counseling may be recommended to help patients adjust to the changes following surgery and to address any emotional or behavioral issues related to eating.
_20240708122007087317__0.webp)